5 Ways Appalachian Healthcare

Introduction to Appalachian Healthcare

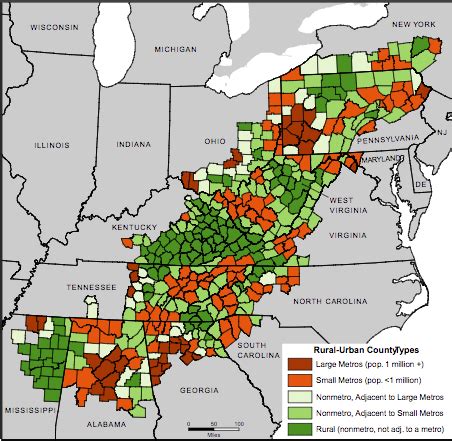
The Appalachian region, spanning across 14 states in the Eastern United States, faces unique healthcare challenges due to its rugged terrain, economic constraints, and limited access to healthcare facilities. Despite these obstacles, the region has made significant strides in improving healthcare outcomes through innovative approaches and community-based initiatives. This article will explore five ways Appalachian healthcare is being transformed to better serve the needs of its residents.
1. Telehealth Services

The use of telehealth services has revolutionized the way healthcare is delivered in Appalachian regions. By leveraging digital technologies such as video conferencing, mobile health applications, and remote monitoring systems, healthcare providers can reach patients in remote areas, reducing the need for in-person visits. This approach has been particularly effective in managing chronic conditions, providing mental health services, and facilitating specialist consultations. Telehealth has not only improved access to care but also helped reduce healthcare disparities in the region.
2. Community-Based Initiatives

Community-based initiatives play a vital role in addressing the healthcare needs of Appalachian residents. These initiatives often involve partnerships between local organizations, healthcare providers, and community leaders to develop targeted programs and services. Some examples include: * Health education and promotion programs * Disease prevention and screening services * Support groups for patients and families * Community-based research and advocacy initiatives These community-driven efforts help build trust, foster engagement, and ensure that healthcare services are tailored to the specific needs of the local population.
3. Workforce Development and Training

The Appalachian region faces significant challenges in recruiting and retaining healthcare professionals, particularly in rural areas. To address this issue, workforce development and training programs have been implemented to support the growth of a skilled and diverse healthcare workforce. These programs include: * Scholarships and loan forgiveness initiatives for healthcare students * Continuing education and professional development opportunities for healthcare professionals * Mentorship and leadership development programs * Recruitment and retention strategies for rural healthcare settings By investing in the development of a strong healthcare workforce, Appalachian regions can ensure that residents have access to high-quality, patient-centered care.
4. Innovative Care Models

Appalachian healthcare is embracing innovative care models that prioritize patient-centered care, population health, and value-based payment. Some examples of these models include: * Accountable Care Organizations (ACOs) * Patient-Centered Medical Homes (PCMHs) * Community Health Worker (CHW) programs * Integrated care models for mental health and substance abuse services These innovative care models focus on delivering high-quality, cost-effective care that addresses the unique needs of Appalachian residents, while also promoting health equity and social determinants of health.
5. Health Equity and Social Determinants of Health

Addressing health equity and social determinants of health is critical to improving healthcare outcomes in Appalachian regions. This involves recognizing the impact of socioeconomic factors, such as poverty, education, and housing, on health status and access to care. Strategies to address health equity and social determinants of health include: * Community-based initiatives to address food insecurity and nutrition * Housing and environmental health programs * Education and job training initiatives * Policy advocacy to address systemic barriers to healthcare access By acknowledging the interconnectedness of health and social determinants, Appalachian healthcare can work towards creating a more equitable and just healthcare system.
💡 Note: The success of these initiatives depends on the collaboration and commitment of local stakeholders, healthcare providers, and community leaders to address the unique challenges and opportunities in Appalachian healthcare.
In summary, Appalachian healthcare is being transformed through the adoption of telehealth services, community-based initiatives, workforce development and training, innovative care models, and a focus on health equity and social determinants of health. These approaches have the potential to improve healthcare outcomes, reduce disparities, and promote health equity in the region. By building on these successes and addressing the ongoing challenges, Appalachian healthcare can continue to evolve and better serve the needs of its residents.
What are the main challenges facing Appalachian healthcare?

+
The main challenges facing Appalachian healthcare include limited access to healthcare facilities, economic constraints, and a shortage of healthcare professionals, particularly in rural areas.
How can telehealth services improve healthcare outcomes in Appalachian regions?
+
Telehealth services can improve healthcare outcomes in Appalachian regions by increasing access to care, reducing travel times and costs, and facilitating specialist consultations and chronic disease management.
What role do community-based initiatives play in addressing healthcare needs in Appalachian regions?
+
Community-based initiatives play a vital role in addressing healthcare needs in Appalachian regions by developing targeted programs and services, building trust and engagement, and ensuring that healthcare services are tailored to the specific needs of the local population.
Related Terms:
- Lexington
- Appalachian Regional healthcare locations
- Appalachian Regional Healthcare careers
- Appalachian regional healthcare middlesboro KY
- appalachian regional health care headquarters
- appalachian regional health care



