Health
5 Tips CareSource EDI

Introduction to CareSource EDI
CareSource is a non-profit health plan that offers a range of health insurance products, including Medicaid, Medicare, and Marketplace plans. To facilitate efficient and secure exchange of health care data, CareSource utilizes Electronic Data Interchange (EDI). EDI is the electronic exchange of business documents, such as claims, eligibility inquiries, and claim status requests, between trading partners. In this article, we will explore 5 tips for working with CareSource EDI.
Tip 1: Understand CareSource EDI Requirements
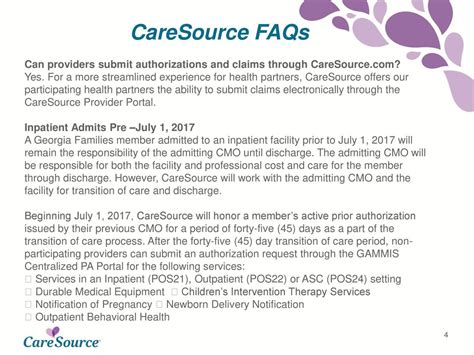
To successfully exchange data with CareSource, it is essential to understand their EDI requirements. This includes familiarizing yourself with the EDI transaction sets and segments used by CareSource, such as the 837 claim transaction and the 835 remittance advice transaction. Additionally, you must ensure that your EDI system is compatible with CareSource’s EDI platform and that you have the necessary credentials to access their system.
Tip 2: Choose the Right EDI Connection Method
CareSource offers several methods for connecting to their EDI system, including:
- Direct Connection: This method involves establishing a direct connection to CareSource’s EDI system using a VPN or AS2 connection.
- Value-Added Network (VAN): This method involves using a third-party VAN to connect to CareSource’s EDI system.
- Clearinghouse: This method involves using a clearinghouse to connect to CareSource’s EDI system.
Tip 3: Test Your EDI Connection

Once you have established your EDI connection, it is crucial to test it to ensure that data is being exchanged correctly. This includes testing your connection with a sample file and verifying that the data is being received and processed correctly by CareSource.
💡 Note: Testing your EDI connection can help identify and resolve any issues before they become major problems.
Tip 4: Use EDI Transactions to Streamline Claims Processing

CareSource EDI supports several transactions that can help streamline claims processing, including:
- 837 Claim Transaction: This transaction is used to submit claims to CareSource.
- 835 Remittance Advice Transaction: This transaction is used to receive payment information from CareSource.
- 276 Claim Status Request Transaction: This transaction is used to inquire about the status of a claim.
Tip 5: Stay Up-to-Date with CareSource EDI Changes

CareSource regularly updates their EDI system and requirements, so it is essential to stay informed about these changes. This includes:
- Subscribing to CareSource’s EDI newsletter or update notifications.
- Attending EDI training sessions or webinars offered by CareSource.
- Regularly reviewing CareSource’s EDI website or portal for updates and changes.
Conclusion Summary
In summary, working with CareSource EDI requires understanding their EDI requirements, choosing the right connection method, testing your connection, using EDI transactions to streamline claims processing, and staying up-to-date with CareSource EDI changes. By following these 5 tips, you can ensure efficient and secure exchange of health care data with CareSource.
What is CareSource EDI?

+
CareSource EDI is the electronic exchange of business documents, such as claims, eligibility inquiries, and claim status requests, between trading partners.
What are the benefits of using CareSource EDI?

+
The benefits of using CareSource EDI include increased efficiency, reduced manual processing, and improved claims processing accuracy.
How do I get started with CareSource EDI?
+
To get started with CareSource EDI, you will need to establish a connection with CareSource’s EDI system, obtain the necessary credentials, and test your connection.
Related Terms:
- CareSource Ohio eligibility requirements
- CareSource Ohio Payer ID
- CareSource Ohio claims address
- CareSource Ohio Provider phone number
- CareSource Login
- Apply for CareSource Ohio



