Change Healthcare Data Breach Notification
Introduction to Change Healthcare Data Breach Notification

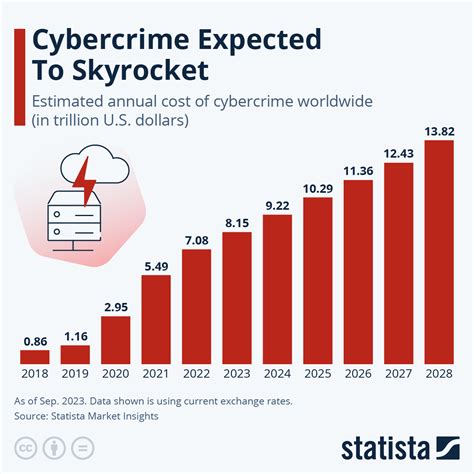
In today’s digital age, the importance of securing sensitive information, especially in the healthcare sector, cannot be overstated. The Health Insurance Portability and Accountability Act (HIPAA) mandates that covered entities and their business associates notify individuals, the Secretary of the U.S. Department of Health and Human Services (HHS), and, in certain circumstances, the media, following a breach of unsecured protected health information (PHI). Change Healthcare, a major player in the healthcare technology and services industry, has been at the forefront of dealing with such breaches, emphasizing the need for robust security measures to protect patient data.
Understanding the Requirements for Breach Notification

The HIPAA Breach Notification Rule requires covered entities to notify affected individuals and the HHS Secretary without unreasonable delay and in no case later than 60 days following the discovery of a breach. If the breach affects 500 or more individuals, the entity must also notify the media. For breaches affecting fewer than 500 individuals, the covered entity must maintain a log of such breaches and notify the HHS Secretary within 60 days of the end of the calendar year. Timely notification is crucial, allowing affected individuals to take steps to protect themselves from potential harm resulting from the breach.
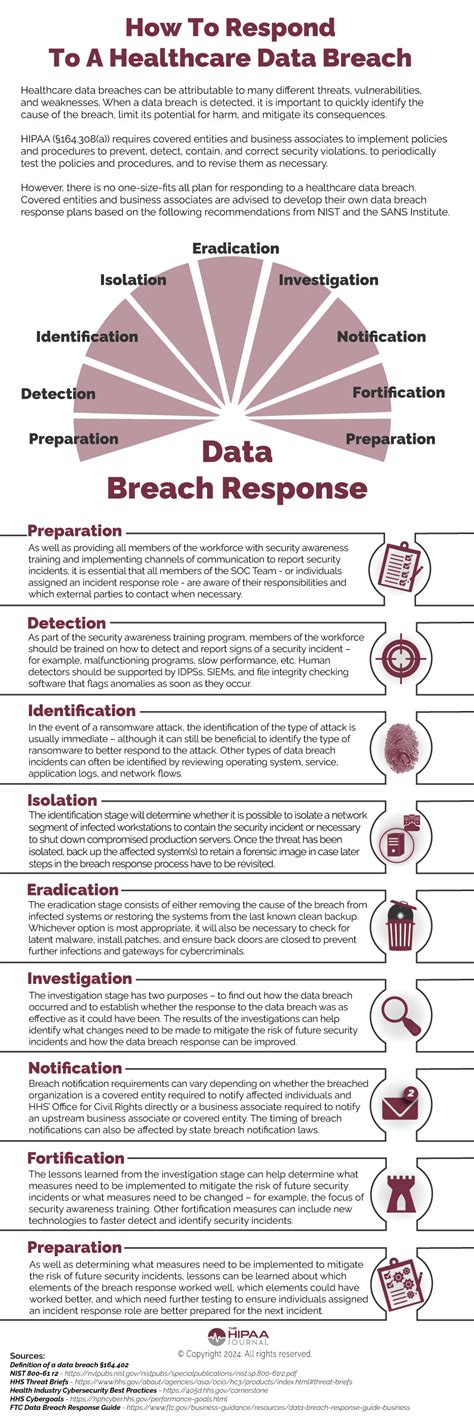
Steps Involved in Notifying a Data Breach
Notifying a data breach involves several key steps: - Identification of the Breach: Determining what constitutes a breach under HIPAA rules. - Investigation: Conducting a thorough investigation to determine the scope of the breach, including the types of PHI involved and the individuals affected. - Risk Assessment: Assessing the risk of harm to affected individuals. - Notification: Providing notice to affected individuals, the HHS, and, when appropriate, the media, in accordance with the timing and content requirements of the HIPAA Breach Notification Rule. - Prevention of Future Breaches: Implementing measures to prevent similar breaches from occurring in the future.
Best Practices for Preventing Data Breaches
Preventing data breaches requires a proactive approach, including: - Regular Security Audits: Conducting regular audits to identify vulnerabilities in the system. - Employee Training: Educating employees on the importance of data security and the procedures for handling PHI. - Encryption: Ensuring that all PHI is encrypted, both in transit and at rest. - Access Controls: Implementing strict access controls to limit who can view or modify PHI. - Incident Response Plan: Having a comprehensive incident response plan in place to quickly respond to and contain breaches.
Consequences of Non-Compliance

Failure to comply with the HIPAA Breach Notification Rule can result in significant financial penalties, with fines ranging from 100 to 50,000 per violation, up to a maximum of $1.5 million per year for each type of violation. Additionally, non-compliance can damage an organization’s reputation and erode patient trust.
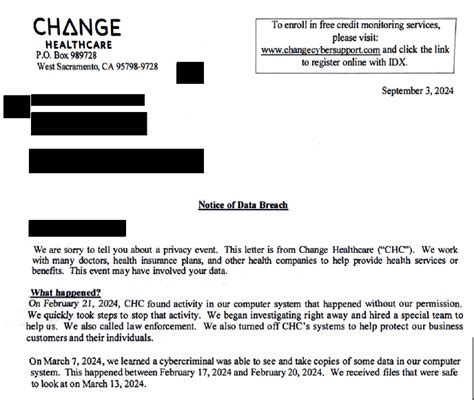
Case Study: Change Healthcare’s Approach

Change Healthcare has been at the forefront of dealing with data breaches, emphasizing the importance of a swift and transparent response. By prioritizing patient privacy and adhering strictly to HIPAA guidelines, Change Healthcare demonstrates a commitment to protecting sensitive healthcare information. This approach includes immediate notification of affected parties, a thorough investigation into the breach, and the implementation of additional security measures to prevent future incidents.
Table of Breach Notification Timeline

| Event | Timeline |
|---|---|
| Discovery of a Breach | Day 0 |
| Investigation and Risk Assessment | Days 1-60 |
| Notification of Affected Individuals | No later than 60 days after discovery |
| Notification of HHS (for breaches affecting 500 or more individuals) | No later than 60 days after discovery |
| Annual Notification to HHS (for breaches affecting fewer than 500 individuals) | Within 60 days of the end of the calendar year |
📝 Note: Understanding and adhering to these timelines is crucial for compliance with the HIPAA Breach Notification Rule.
In the aftermath of a data breach, the focus shifts towards recovery and prevention. Implementing stronger security measures, enhancing employee training, and regularly updating policies and procedures can help mitigate the risk of future breaches. The healthcare industry’s shift towards digital records and telehealth services underscores the need for robust data protection strategies.
As the healthcare landscape continues to evolve, the importance of protecting patient data will only continue to grow. By prioritizing data security, adhering to regulatory requirements, and adopting best practices for breach notification and prevention, healthcare organizations can safeguard patient trust and ensure compliance with stringent data protection laws.
In essence, navigating the complexities of data breach notification in healthcare requires a deep understanding of regulatory requirements, a proactive approach to security, and a commitment to transparency and patient privacy. By embracing these principles, healthcare organizations can foster a culture of compliance and security, ultimately protecting the sensitive information that is entrusted to them.
What is the primary goal of the HIPAA Breach Notification Rule?
+
The primary goal of the HIPAA Breach Notification Rule is to ensure that individuals whose protected health information (PHI) has been compromised are notified promptly, allowing them to take protective measures against potential identity theft or other harms.
How long does a covered entity have to notify affected individuals of a breach?
+
A covered entity must notify affected individuals without unreasonable delay and in no case later than 60 days following the discovery of a breach.
What are the consequences for non-compliance with the HIPAA Breach Notification Rule?
+
Non-compliance can result in significant financial penalties, ranging from 100 to 50,000 per violation, up to a maximum of $1.5 million per year for each type of violation, as well as damage to the organization’s reputation and patient trust.
Related Terms:
- change health care cybersecurity breach
- change health care breach notification



