5 Behavioral Health Regulations
Introduction to Behavioral Health Regulations
The landscape of behavioral health is complex and heavily regulated to ensure the provision of high-quality, patient-centered care. These regulations span various aspects, from privacy and confidentiality to treatment standards and insurance coverage. Understanding these regulations is crucial for healthcare providers, policymakers, and patients alike, as they form the foundation upon which effective, compassionate care is delivered. This article will delve into five key behavioral health regulations, exploring their implications and the importance of compliance.
1. Health Insurance Portability and Accountability Act (HIPAA)
The Health Insurance Portability and Accountability Act (HIPAA) is a cornerstone of healthcare regulations in the United States. Enacted in 1996, HIPAA includes provisions to protect the privacy and security of patient health information. For behavioral health providers, HIPAA compliance is particularly stringent due to the sensitive nature of the information involved. This includes ensuring that all electronic protected health information (ePHI) is encrypted, that access to patient records is strictly controlled, and that patients are informed of their rights regarding their health information. HIPAA violations can result in significant fines, making compliance a top priority for all healthcare providers.
2. Mental Health Parity and Addiction Equity Act (MHPAEA)
The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 is a federal law that requires health insurance plans to provide equal coverage for mental health and substance use disorders as they do for medical and surgical care. This law was a significant step towards reducing the disparities in insurance coverage that have historically affected individuals seeking mental health and addiction treatment. By ensuring parity, MHPAEA aims to increase access to necessary care, reduce discrimination, and promote overall health and wellbeing. Compliance with MHPAEA involves insurers and healthcare providers ensuring that their policies and practices do not unfairly limit or exclude coverage for mental health and addiction services.
3. 42 CFR Part 2
42 CFR Part 2 is a federal regulation that protects the confidentiality of substance use disorder patient records. These regulations are more stringent than HIPAA in several key areas, reflecting the unique challenges and vulnerabilities associated with substance use disorders. For instance, 42 CFR Part 2 generally requires patient consent before disclosure of records for purposes not directly related to treatment, and it imposes specific requirements for the disclosure of patient information in legal proceedings. Compliance with 42 CFR Part 2 is essential for providers of substance use disorder services to maintain patient trust and ensure that individuals feel safe seeking help without fear of stigma or repercussions.
4. Americans with Disabilities Act (ADA)
The Americans with Disabilities Act (ADA) prohibits discrimination against individuals with disabilities, including those with mental health and substance use disorders, in all areas of public life, including jobs, schools, transportation, and all public and private places that are open to the general public. For behavioral health providers, ADA compliance involves ensuring that their facilities, services, and programs are accessible to individuals with disabilities. This can include providing accommodations such as sign language interpreters, readers, or other auxiliary aids for patients who are deaf or hard of hearing, or modifying policies and procedures to avoid discrimination against individuals with mental health conditions.
5. Electronic Visit Verification (EVV)

Electronic Visit Verification (EVV) is a regulation that requires healthcare providers, including those in behavioral health, to use electronic systems to verify the occurrence of home and community-based services (HCBS). The goal of EVV is to reduce fraud and abuse, improve the quality of care, and increase transparency and accountability in healthcare delivery. For behavioral health providers, implementing EVV involves selecting and integrating an EVV system into their operations, training staff, and ensuring that the system is used correctly for all applicable services. Compliance with EVV regulations is mandatory for providers participating in Medicaid, with specific implementation timelines and requirements set by each state.
📝 Note: Compliance with these regulations is not only legally required but also ethically imperative for maintaining patient trust and ensuring the delivery of high-quality care.
In terms of implementation and compliance, the following steps can be taken: - Conduct Regular Audits: To ensure ongoing compliance with regulatory requirements, healthcare providers should conduct regular audits of their policies, procedures, and practices. - Provide Ongoing Training: Staff should receive regular training on the regulations that apply to their roles, including updates on any changes to laws or regulations. - Engage with Regulatory Bodies: Maintaining an open dialogue with regulatory agencies can help providers stay informed about expectations and best practices for compliance.
The regulatory landscape of behavioral health is dynamic, with laws and regulations evolving to address emerging challenges and improve care outcomes. Staying abreast of these changes and prioritizing compliance is essential for providers seeking to deliver effective, patient-centered care.
In reflecting on the regulatory framework surrounding behavioral health, it’s clear that these laws and regulations play a vital role in safeguarding patient rights, promoting access to care, and fostering an environment in which high-quality, compassionate services can thrive. As the field continues to evolve, the importance of these regulations will only continue to grow, underscoring the need for ongoing education, compliance, and advocacy.
What is the primary purpose of HIPAA in behavioral health?
+
The primary purpose of HIPAA is to protect the privacy and security of patient health information, ensuring that sensitive data is handled with care and confidentiality.
How does the Mental Health Parity and Addiction Equity Act impact insurance coverage?
+
The MHPAEA requires health insurance plans to provide equal coverage for mental health and substance use disorders as they do for medical and surgical care, reducing disparities and increasing access to necessary treatments.
What are the key implications of 42 CFR Part 2 for substance use disorder treatment providers?

+
42 CFR Part 2 imposes stringent confidentiality requirements on substance use disorder patient records, mandating consent before disclosure for non-treatment purposes and specifying procedures for legal disclosures, to protect patient privacy and trust.
Related Terms:
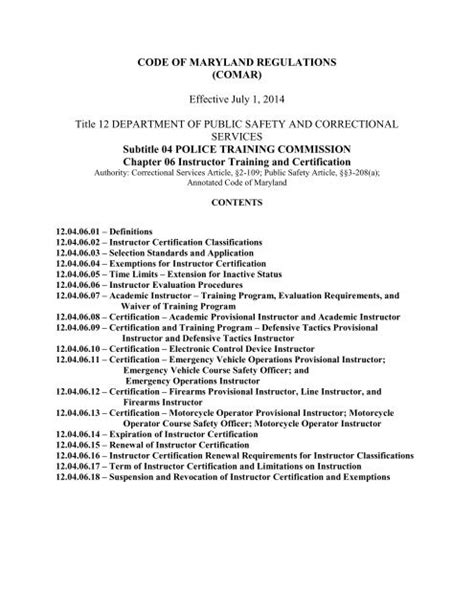
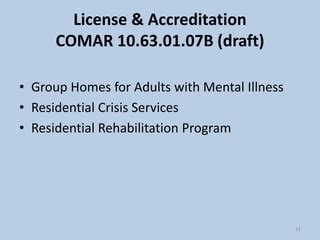
- COMAR 10 63 Regulations
- COMAR Regulations for Behavioral Health
- COMAR regulations for OMHC
- COMAR Regulations for PRP
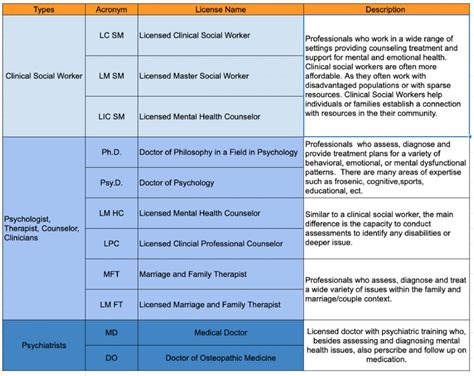
- Behavioral health license types
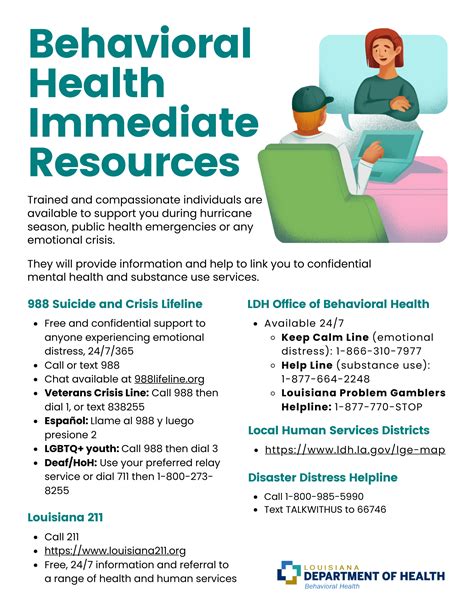
- Behavioral health Authority