Seven Mental Health Subscales Explained
Introduction to Mental Health Subscales
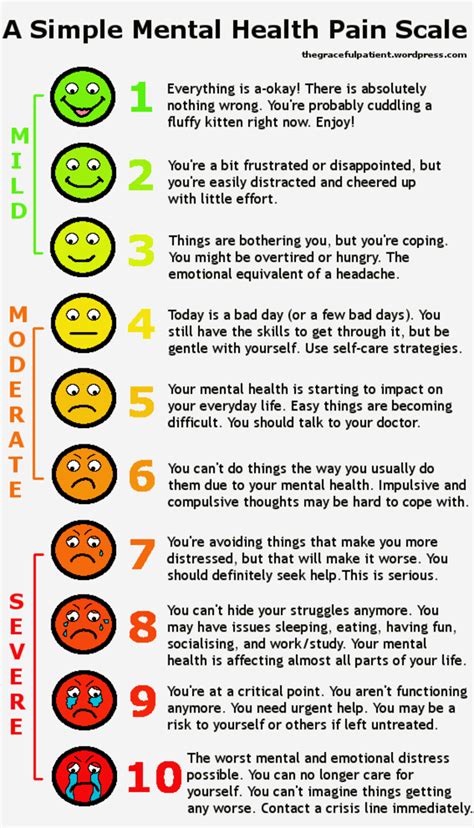
Mental health is a complex and multifaceted aspect of human well-being, encompassing various dimensions that contribute to an individual’s overall psychological state. The World Health Organization (WHO) defines mental health as “a state of well-being in which every individual realizes their own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community.” To better understand and assess mental health, researchers and clinicians often utilize mental health subscales, which are standardized measures designed to evaluate specific aspects of mental health. In this blog post, we will delve into seven mental health subscales, exploring their definitions, applications, and implications for mental health assessment and intervention.
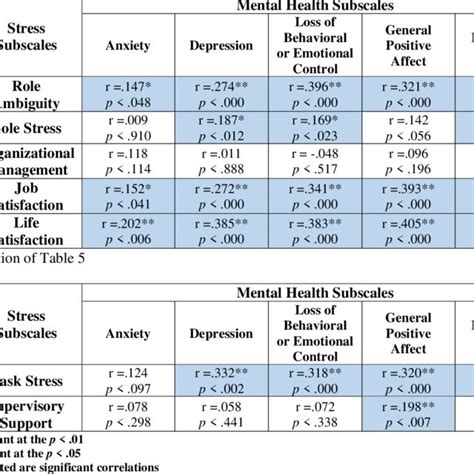
Subscale 1: Anxiety

The anxiety subscale is a widely used measure to assess the level of anxiety an individual experiences. Anxiety is characterized by feelings of worry, nervousness, and fear that are persistent and overwhelming, interfering with daily life. The anxiety subscale typically includes items that evaluate the frequency and intensity of anxiety symptoms, such as fear of the future, worries about everyday things, and physical symptoms like a racing heart. By assessing anxiety levels, mental health professionals can identify individuals who may benefit from anxiety-reducing interventions, such as cognitive-behavioral therapy (CBT) or medication.
Subscale 2: Depression
The depression subscale is another crucial measure in mental health assessment, designed to evaluate the severity of depressive symptoms. Depression is a mood disorder characterized by persistent feelings of sadness, hopelessness, and a lack of interest in activities. The depression subscale typically includes items that assess mood, motivation, and physical symptoms like changes in appetite or sleep patterns. By identifying individuals with elevated depressive symptoms, mental health professionals can provide targeted interventions, such as antidepressant medication or talk therapy, to help alleviate symptoms and improve overall mental health.
Subscale 3: Stress
The stress subscale is used to assess the level of stress an individual experiences in response to life events, relationships, or daily pressures. Stress is a common experience that can have both positive and negative effects on mental health. The stress subscale typically includes items that evaluate perceived stress, coping mechanisms, and physical symptoms like headaches or fatigue. By understanding an individual’s stress levels and coping strategies, mental health professionals can develop stress management plans, such as relaxation techniques or problem-focused coping, to enhance overall well-being.
Subscale 4: Self-Esteem
The self-esteem subscale is a measure of an individual’s overall self-worth and confidence. Self-esteem is a critical aspect of mental health, as it influences how individuals perceive themselves, their relationships, and their place in the world. The self-esteem subscale typically includes items that assess self-perception, confidence, and self-acceptance. By evaluating self-esteem levels, mental health professionals can identify individuals who may benefit from self-esteem enhancing interventions, such as positive self-talk or self-compassion exercises, to promote a more positive and realistic self-image.
Subscale 5: Emotional Regulation
The emotional regulation subscale is designed to assess an individual’s ability to manage and regulate their emotions in response to various situations. Emotional regulation is a vital aspect of mental health, as it influences how individuals respond to stress, relationships, and daily challenges. The emotional regulation subscale typically includes items that evaluate emotional awareness, emotional expression, and emotional control. By understanding an individual’s emotional regulation strategies, mental health professionals can develop targeted interventions, such as mindfulness or emotional labeling, to enhance emotional well-being.
Subscale 6: Social Support
The social support subscale is a measure of the perceived availability and quality of social support from family, friends, and community. Social support is a critical aspect of mental health, as it influences how individuals cope with stress, trauma, and daily challenges. The social support subscale typically includes items that assess perceived support, social connections, and support-seeking behaviors. By evaluating social support levels, mental health professionals can identify individuals who may benefit from social support enhancing interventions, such as social skills training or support group participation, to promote stronger social bonds and a sense of belonging.
Subscale 7: Resilience
The resilience subscale is designed to assess an individual’s ability to bounce back from adversity, trauma, or significant stress. Resilience is a vital aspect of mental health, as it influences how individuals cope with challenges and setbacks. The resilience subscale typically includes items that evaluate coping strategies, stress management, and post-traumatic growth. By understanding an individual’s resilience levels, mental health professionals can develop targeted interventions, such as resilience training or coping skills development, to enhance overall mental health and well-being.
📝 Note: These subscales are not mutually exclusive, and individuals may exhibit symptoms across multiple subscales. A comprehensive mental health assessment should consider the complex interplay between these subscales to provide a nuanced understanding of an individual's mental health.
In terms of applications, mental health subscales can be used in various settings, including: * Clinical practice: to inform diagnosis, treatment planning, and outcome evaluation * Research: to investigate the underlying mechanisms of mental health conditions and develop new interventions * Public health: to monitor population-level mental health trends and develop targeted prevention and intervention strategies
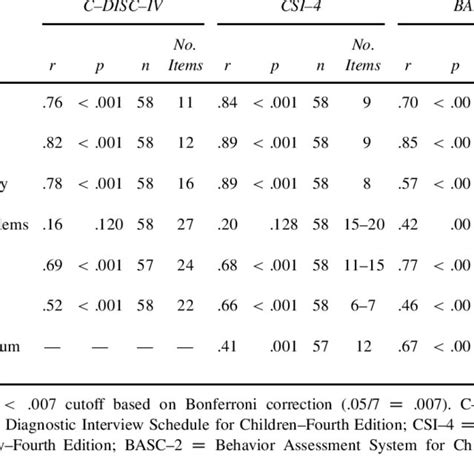
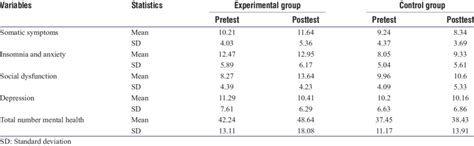
The following table illustrates the seven mental health subscales, their definitions, and examples of assessment items:
| Subscale | Definition | Assessment Items |
|---|---|---|
| Anxiety | Excessive fear or worry | Fear of the future, worries about everyday things, physical symptoms like a racing heart |
| Depression | Persistent feelings of sadness or hopelessness | Mood, motivation, physical symptoms like changes in appetite or sleep patterns |
| Stress | Perceived pressure or tension | Perceived stress, coping mechanisms, physical symptoms like headaches or fatigue |
| Self-Esteem | Overall self-worth and confidence | Self-perception, confidence, self-acceptance |
| Emotional Regulation | Ability to manage and regulate emotions | Emotional awareness, emotional expression, emotional control |
| Social Support | Perceived availability and quality of social support | Perceived support, social connections, support-seeking behaviors |
| Resilience | Ability to bounce back from adversity or trauma | Coping strategies, stress management, post-traumatic growth |
In summary, the seven mental health subscales provide a comprehensive framework for understanding the complex and multifaceted nature of mental health. By assessing these subscales, mental health professionals can develop targeted interventions and support strategies to promote overall mental health and well-being.
What is the purpose of mental health subscales?
+
Mental health subscales are used to assess specific aspects of mental health, providing a comprehensive understanding of an individual’s psychological state and informing diagnosis, treatment planning, and outcome evaluation.
Can mental health subscales be used in combination?

+
Yes, mental health subscales can be used in combination to provide a nuanced understanding of an individual’s mental health, as symptoms often overlap across multiple subscales.
How can mental health subscales be applied in real-world settings?
+
Mental health subscales can be applied in clinical practice, research, and public health settings to inform diagnosis, treatment planning, and prevention strategies, ultimately promoting overall mental health and well-being.