5 Soap Note Examples
Introduction to Soap Notes
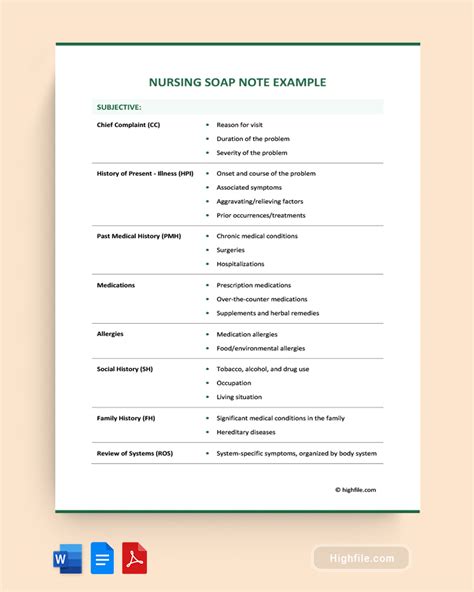
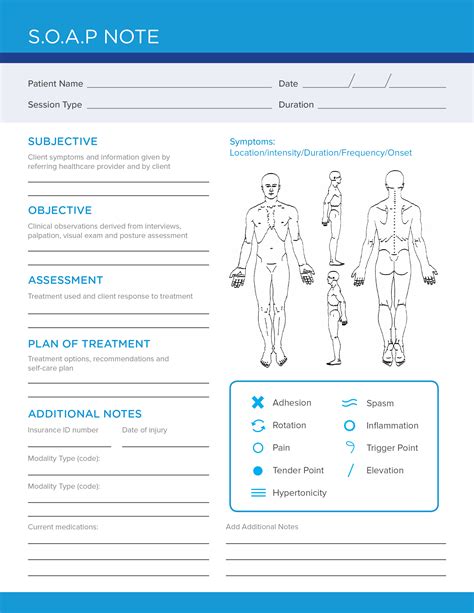
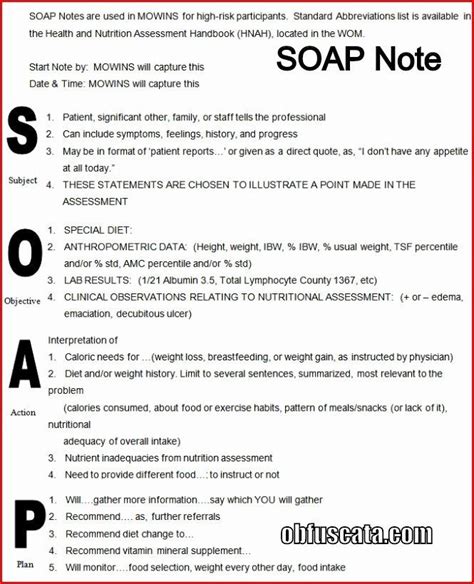
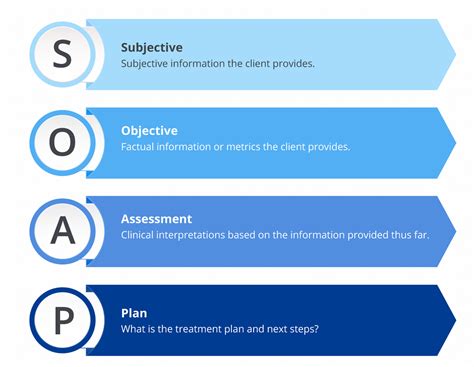
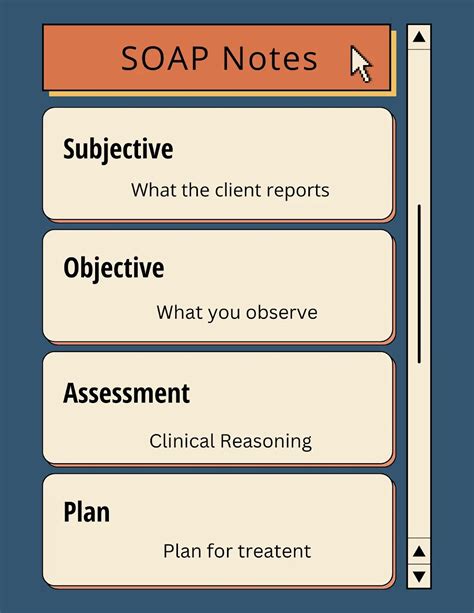
Soap notes are a type of documentation used by healthcare professionals to record patient information in a structured and organized manner. The acronym “SOAP” stands for Subjective, Objective, Assessment, and Plan, which are the four main components of a soap note. In this article, we will explore five different soap note examples to illustrate how they are used in various medical scenarios.
What are Soap Notes?
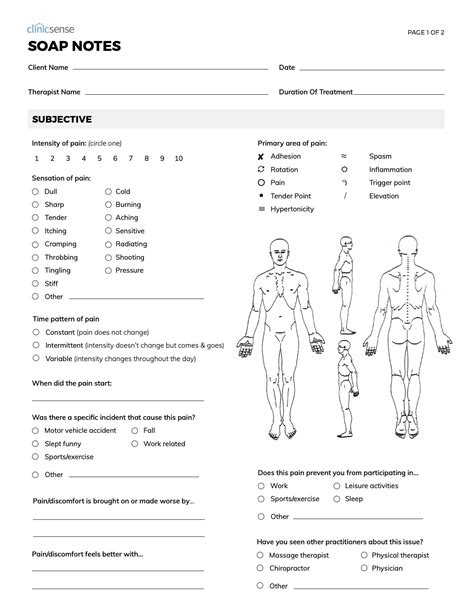
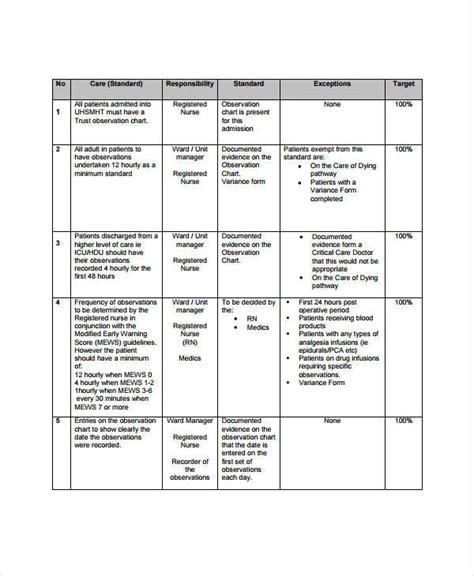
Soap notes are a crucial part of patient care, as they provide a clear and concise record of a patient’s medical history, current symptoms, and treatment plan. They are used by healthcare professionals, such as doctors, nurses, and therapists, to communicate effectively and ensure continuity of care. Soap notes are typically used in outpatient and inpatient settings, and are an essential tool for healthcare providers to track patient progress and make informed decisions about treatment.
Example 1: Soap Note for a Patient with Diabetes
The following is an example of a soap note for a patient with diabetes:
- Subjective: The patient reports feeling fatigued and experiencing increased thirst and urination over the past few days.
- Objective: The patient’s blood glucose level is 250 mg/dL, and their blood pressure is 140⁄90 mmHg.
- Assessment: The patient is diagnosed with uncontrolled diabetes mellitus.
- Plan: The patient will be started on metformin 500 mg twice daily, and will be advised to monitor their blood glucose levels closely and follow a healthy diet and exercise plan.
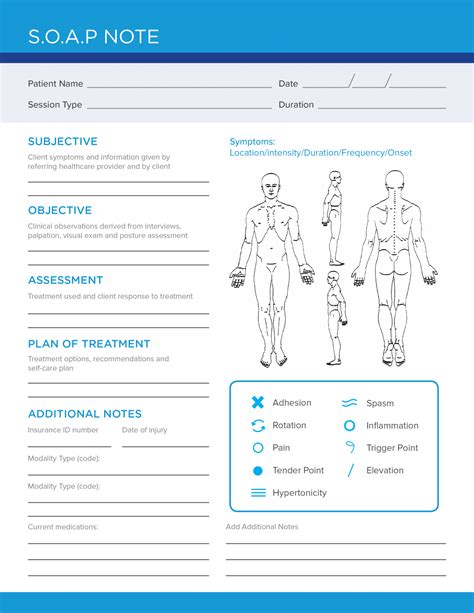
Example 2: Soap Note for a Patient with a Broken Arm
The following is an example of a soap note for a patient with a broken arm:
- Subjective: The patient reports feeling severe pain and limited mobility in their arm after a fall.
- Objective: The patient’s X-ray shows a fracture of the humerus, and their arm is swollen and bruised.
- Assessment: The patient is diagnosed with a fractured humerus.
- Plan: The patient will be treated with a cast and pain medication, and will be advised to follow up with an orthopedic specialist for further evaluation and treatment.
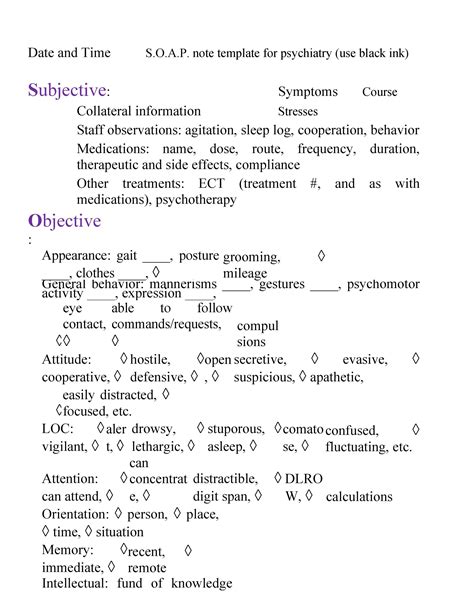
Example 3: Soap Note for a Patient with Anxiety
The following is an example of a soap note for a patient with anxiety:
- Subjective: The patient reports feeling anxious and overwhelmed, and is experiencing difficulty sleeping and concentrating.
- Objective: The patient’s vital signs are within normal limits, but they appear anxious and fidgety during the examination.
- Assessment: The patient is diagnosed with anxiety disorder.
- Plan: The patient will be started on a selective serotonin reuptake inhibitor (SSRI) and will be advised to engage in relaxation techniques, such as deep breathing and meditation, to manage their anxiety symptoms.
Example 4: Soap Note for a Patient with Hypertension
The following is an example of a soap note for a patient with hypertension:
- Subjective: The patient reports feeling dizzy and lightheaded, and is experiencing frequent headaches.
- Objective: The patient’s blood pressure is 180⁄100 mmHg, and their electrocardiogram (ECG) shows left ventricular hypertrophy.
- Assessment: The patient is diagnosed with uncontrolled hypertension.
- Plan: The patient will be started on a diuretic and an ACE inhibitor, and will be advised to monitor their blood pressure closely and follow a healthy diet and exercise plan.
Example 5: Soap Note for a Patient with a Respiratory Infection
The following is an example of a soap note for a patient with a respiratory infection:
- Subjective: The patient reports feeling short of breath and experiencing a productive cough.
- Objective: The patient’s lung exam shows decreased breath sounds and wheezing, and their chest X-ray shows pulmonary infiltrates.
- Assessment: The patient is diagnosed with a respiratory infection.
- Plan: The patient will be started on antibiotics and will be advised to rest, stay hydrated, and use a humidifier to manage their symptoms.
📝 Note: Soap notes are an essential part of patient care, and healthcare providers should strive to make them as detailed and accurate as possible to ensure the best possible outcomes for their patients.
In summary, soap notes are a crucial part of patient care, and are used by healthcare professionals to document patient information in a structured and organized manner. The five examples provided in this article illustrate how soap notes are used in various medical scenarios, and demonstrate the importance of accurate and detailed documentation in ensuring the best possible outcomes for patients.
What is the purpose of a soap note?
+
The purpose of a soap note is to provide a clear and concise record of a patient’s medical history, current symptoms, and treatment plan.
What are the four main components of a soap note?
+
The four main components of a soap note are Subjective, Objective, Assessment, and Plan.
How are soap notes used in patient care?
+
Soap notes are used by healthcare professionals to communicate effectively and ensure continuity of care. They provide a clear and concise record of a patient’s medical history, current symptoms, and treatment plan, and are an essential tool for healthcare providers to track patient progress and make informed decisions about treatment.
Related Terms:
- Nursing SOAP notes examples
- SOAP notes PDF
- SOAP note example Nurse Practitioner
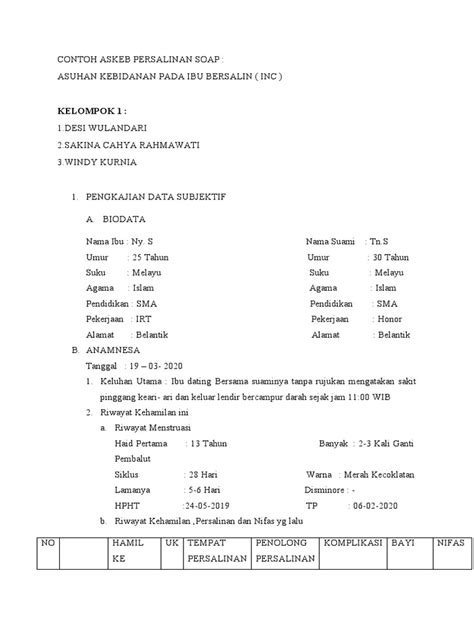
- Soap notes contoh
- SOAP notes meaning
- soap method medical charting